Can Sinusitis Cause Sleep Apnea?
Sleep apnea and sinusitis are distinctly different medical conditions, however both can affect breathing and quality of sleep and an increasing body of peer reviewed medical research is emerging that points to a potential link between the two.
Sinusitis is a condition that describes the inflammation or swelling of the sinuses, leading to nasal congestion or nasal stuffiness. The symptoms of sinusitis and resulting congestion of the nasal passages can lead to breathing issues and sinusitis itself can often be caused by underlying bacterial or viral infection. Recurrent sinus infections can also be experienced due to structural abnormalities such as a deviated septum as well as medical issues that affect the immune system.
Sleep apnea is sometimes confused with snoring, but it is actually a lot more serious. It is a sleeping disorder that can have serious effects on your overall health and wellbeing as well as on your ability to sleep.
People who suffer with recurrent sinusitis often have trouble breathing easily when they sleep and in this article we will look at the exact relationship between sinusitis and sleep apnea. We will also provide people suffering with sinusitis with some tips to help get a full night of sleep.
Understanding Sinusitis
What is Sinusitis?
There are air-filled spaces in the bones of the face and skull that are known as sinus cavities which can swell. The sinus cavities are lined with tissue that is known as sinus mucosa, which are responsible for the production of mucus that plays an important role of controlling the filtration and humidity of the air we breathe.
Inflammation of the sinus mucosa is what we refer to as Sinusitis, causing the congestion and discomfort and other symptoms that we often associated with the condition.
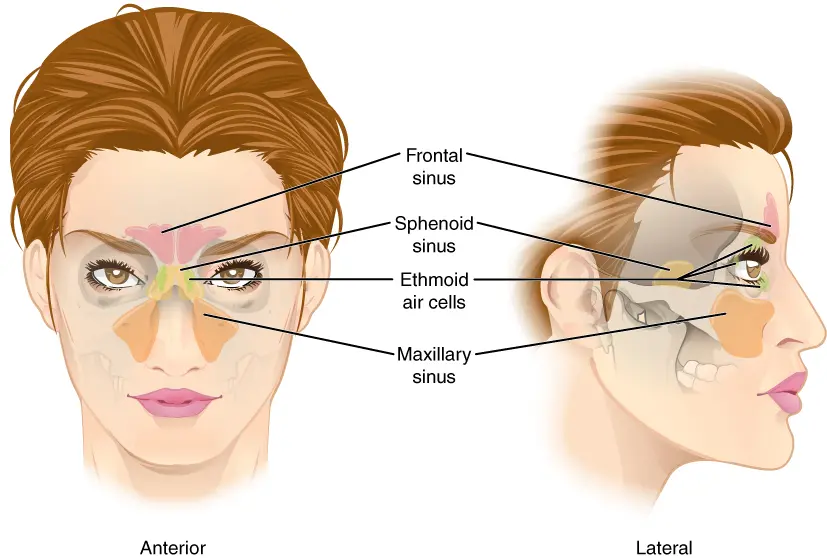
The Functions of the Sinus Cavities
Each sinus cavity comes in pairs, there are four of them which you can see in the image. Located in the forehead, cheeks behind the nose and between the eyes, each sinus cavity has its own function which range from improving vocal resonance, acting as a buffer to reduce facial trauma or managing the weight of the skull.
When the sinuses are blocked or infected, they can cause significant discomfort and their normal function can be impaired. A study published in the Laryngoscope Investigative Otolaryngology even found compelling evidence of a link between sinusitis and balance disorders, with sufferers of chronic sinusitis showing a higher prevalence of balance impairment when compared to the control group.
Other research published by journals such as Rhinology and the JAMA Otolaryngology-Head & Neck Surgery looked at the link between chronic rhinosinusitis (which is when sinusitis symptoms persist for 12 weeks more despite attempts to treat it) and mental health, finding a higher prevalence of anxiety and depression when compared to the control group, and in the latter cited research they found that surgery to treat this condition led to patients experiencing significant improvements in depression and overall mental health.
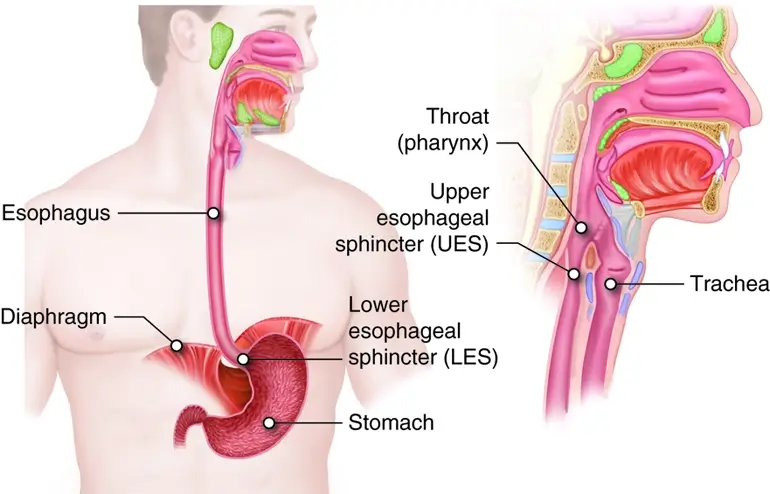
The Link Between The Sinus Cavities and the Upper Respiratory System
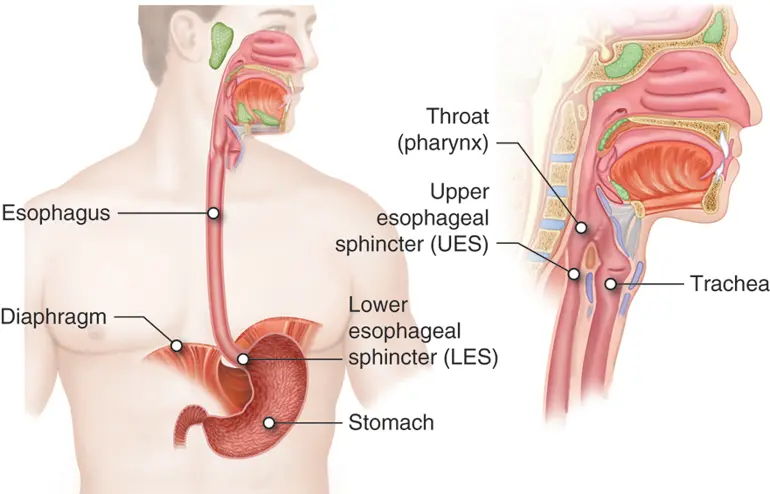
The sinuses are interconnected with the respiratory system, in particular the upper respiratory system, including the nose and throat. As mentioned previously, the nasal passages work together to produce mucus that helps to filter the air we breathe from foreign particles and airborne pathogens. The sinus is your first filter and line of defense, which is why when they are inflamed the intricate system is disrupted and potential complications and other symptoms can arise.
The Role of Mucus in Sinus Passages
Mucus is often the first thing most people associate with a cold or flu, especially when said mucus is colored green. It is, however, a critical part of the body's respiratory system and a defense mechanism that protects us in quite a few ways.
Mucus helps to keep the nasal passages and sinuses moist, which allows them to function efficiently. It also helps to trap irritants and foreign particles including allergens before they can enter the lungs.
When the lining of the sinus becomes inflamed, the body overproduces mucus and this excess can accumulate in the sinuses, impairing drainage and helping to create an environment that promotes the growth of bacterial infection and viral infectious diseases.
Acute Sinusitis, Subacute Sinusitis and Chronic Sinusitis
Sinusitis is usually classified by the duration and severity of the symptoms, there are two principal categories which are acute sinusitis and chronic sinusitis, however there is also an intermediate type which is known as subacute sinusitis.
Acute Sinusitis Symptoms
Acute sinusitis is the most commonly occurring type, lasting for less than 4 weeks and is often a result of viral infection, such as a common cold. The symptoms can include nasal congestion, facial pain or pressure, runny nose and postnasal drip. As mentioned this type of sinus infection lasts for no more than four weeks.
Subacute Sinusitis
This intermediate form form of sinus infection lasts between four and twelve weeks. The causes can vary and include bacterial infection and viral infection. When symptoms of sinusitis persist for more than four weeks, medical evaluation is recommended and medical intervention may be required.
Chronic Sinusitis
When the symptoms of sinus infection last for longer than twelve weeks it can be due to ongoing inflammation rather than an acute infection. This can significantly impair quality of life, cause facial pain and excessive mucus for an extended period of time.
Most often this type of sinus infections happen when underlying factors such as nasal polyps, deviated nasal septum or persistent allergies. This type of sinusitis often requires medical intervention in the form of medication or surgery in order to effectively address it, an ENT expert or allergy specialist can take actions such as prescribing antibiotics or nasal sprays to help reduce the inflammation in tissue lining.
Causes and Risk Factors of Sinusitis
There are a number of causes and risk factors for sinusitis, some of the key factors include:
- Nasal Polyps
Nasal polyps are non-cancerous growths that develop in the nasal passages or sinuses. As you can imagine they can become obstructive and start negatively affecting the drainage, contributing to chronic inflammation which leads to sinus infections and acute sinusitis. - Deviated Nasal Septum
As we have previously discussed, the nasal septum is the thin wall that separates the nostrils, when this is displaced or lopsided, it can deviate the airflow causing obstruction and hindering proper drainage, again increasing the risk of sinus infection sinusitis. A deviated nasal septum can be identified by a qualified ear nose and throat specialist such as the team at our ENT Clinic in Dubai. - Allergies
Allergies can trigger a variety of responses in people hat range from a runny nose to swollen nasal passages and nose pain. Allergic rhinitis, commonly called hayfever, can be triggered by allergens such as pollen, dust mites or even pet hair. These allergies can cause nasal inflammation and congestion, increasing the risk of sinus infection.
MEET OUR ENT & PLASTIC SURGERY TEAM
- All
- ENT
- Plastic Surgery

- Weakened Immune System
When someone has a weakened immune system they are at a higher risk of infections, including sinusitis. This is because the immune system will have a harder time in fighting off pathogens which can lead to recurrent or chronic sinus infections.
- Upper Respiratory Infections
The upper respiratory tract can become infected, this often takes the form of the common cold or influenza. These infections can precede or accompany sinusitis and are often viral in nature, leading to inflammation and congestion in nasal passages and sinuses that helps promote bacterial growth. and bacterial sinus infections.
What is Sleep Apnea?
You might think of sleep apnea as snoring, many people confuse the two, however sleep apnea is more serious. It is a medically recognised sleep disorder that causes interruptions in breathing during sleep. These interruptions, called apneas, can last for several seconds to minutes and can occur multiple times throughout the night. There are three main types of sleep apnea:
- Obstructive Sleep Apnea (OSA)
The airway becomes partially or completely blocked during sleep, usually because the throat muscles have relaxed or the tonsils are enlarged or there is excess tissue in the throat. - Central Sleep Apnea (CSA)
Caused by a failure of the brain to send proper signals to the muscles that control breathing during sleep. - Complex Sleep Apnea Syndrome (CSAS)
A combination of both obstructive and central sleep apnea.
Impact of Sleep Apnea on Overall Health
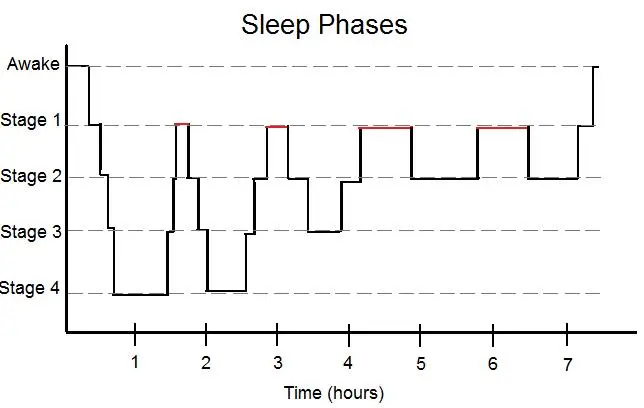
Repeated interruptions in breathing during sleep can lead to fragmented and poor-quality sleep, resulting in daytime sleepiness, fatigue, and impaired cognitive function. Your body needs to enter into the REM state of deep sleep in order to recuperate fully, this usually happens in cycles of 80-100 minutes.
Sleep apnea can also contribute to the development or worsening of various medical conditions, including:
- High Blood Pressure
There is a strong proven link between sleep disordered breathing and hypertension (high blood pressure), it is thought this is because of the frequent episodes of oxygen deprivation during sleep which can cause blood pressure to rise, increasing the risk of cardiovascular problems. - Heart Disease
Sleep apnea has been found in medical research to be associated with an increased risk of heart disease, including heart attacks, irregular heart rhythms (arrhythmias), and heart failure. The mechanisms underlying this relationship are still being studied but may involve inflammation, oxidative stress, and endothelial dysfunction. - Stroke
Research has shown that sleep apnea increases the risk of stroke. The repeated pauses in breathing can lead to decreased oxygen levels and increased carbon dioxide levels, which can negatively impact the cardiovascular system and increase the likelihood of stroke. - Type 2 Diabetes
Sleep apnea has been linked to an increased risk of developing type 2 diabetes. The disrupted sleep patterns and intermittent hypoxia associated with sleep apnea can contribute to insulin resistance and impaired glucose metabolism.
Research on Sinusitis and Sleep Apnea
Research suggests a potential link between sleep apnea and sinusitis, although the exact nature of this relationship is still being explored. Both conditions share certain risk factors, such as nasal congestion, chronic inflammation, and compromised immune function, which may contribute to their co-occurrence.
In individuals with sleep apnea, the recurring episodes of airway obstruction and reduced airflow can lead to nasal congestion and inflammation. This nasal congestion may impede proper sinus drainage, creating an environment that is more susceptible to sinus infections.
Repetitive breathing pauses and the resulting low oxygen levels during sleep apnea can lead to tissue inflammation and compromise immune responses. These factors may contribute to an increased susceptibility to sinus infections or exacerbation of existing sinusitis.
Further research is needed to fully elucidate the relationship between sleep apnea and sinusitis. However, it is important for individuals with sleep apnea to be aware of the potential impact on their sinus health and seek appropriate medical attention if sinus symptoms arise.
Scientific Studies and Findings
Scientific research has focused on understanding the relationship between sinusitis and sleep apnea. Several studies have shed light on the potential associations and shared risk factors between these two conditions.
A study published in the journal Sleep Medicine looked at the incidence of sinusitis in individuals with obstructive sleep apnea. The researchers found a higher incidence of chronic sinusitis in patients with sleep apnea compared to the general population.
They hypothesized that the recurrent airway obstructions and subsequent nasal congestion in sleep apnea may contribute to the development or persistence of sinusitis.
Another study published in the American Journal of Rhinology & Allergy explored the impact of continuous positive airway pressure (CPAP) therapy, a common treatment for sleep apnea, on sinus symptoms.
The researchers found that CPAP therapy led to improvements in nasal congestion and sinusitis symptoms in patients with sleep apnea. The findings suggested a potential link between sleep apnea treatment and sinus health.
These studies, along with others in the field, provide valuable insights into the potential connections between sinusitis and sleep apnea. They highlight the need for further research to fully understand the underlying mechanisms and develop effective management strategies for individuals with both conditions.
Managing Sinusitis & Sleep Apnea
Addressing Sleep Apnea
You can aim to improve the quality of sleep, we recommend seeing an ENT expert who might be able to assist with advice on the best possible therapy or treatment. These can include things like a machine that delivers a continuous flow of air that keeps your airway open, known as CPAP therapy.

Other forms of treatment can include oral devices and in some cases surgeries such as nasal septoplasty, turbinate reduction or uvulopalatopharyngoplasty (UPPP). The choice of treatment will depend things like the severity and type of the condition and individual patient circumstances.
Tips to Prevent Sinus Infections
People can be more at risk to sinus infection at certain times, for example some people might suffer from sinusitis after a long international flight, a condition known as aerosinusitis. Other times might include when your immune system is down, such as after an extended period of poor sleep and diet, other illnesses etc.
Taking precautions against the onset of sinusitis might include using nasal sprays to help reduce inflammation in the nasal passages, promoting proper drainage and alleviating symptoms.
Rinsing the nasal passages with nasal irrigation using a nasal irrigator can help to flush out excess mucus from the sinuses. There are nasal sprays that are prescribed by doctors which are often called steroid nasal sprays, and there are over the counter ones such as Otravine which have Xylometazoline Hydrochloride as the active ingredient.
For chronic or recurrent sinusitis that does not respond to medical treatment, further interventions may be considered. These can include referral to an ear, nose, and throat specialist for further evaluation and management.
Conclusion
The potential link between sinusitis and sleep apnea lies in shared risk factors, including nasal congestion, inflammation, and compromised immune function. Managing both conditions effectively requires a comprehensive approach that addresses underlying causes and promotes overall sinus and sleep health.
Here are some key takeaways to improve the quality of sleep and sinus health:
Maintain good sleep hygiene
Establish a regular sleep schedule, create a comfortable sleep environment, and practice relaxation techniques before bed to promote restful sleep.
Seek medical evaluation: If you suspect you have sinusitis or sleep apnea, consult with healthcare professionals who specialize in ear, nose, and throat or sleep medicine for an accurate diagnosis and tailored treatment plan.
Treat sinusitis promptly: If you experience symptoms of sinusitis, such as facial pain, nasal congestion, or postnasal drip, seek appropriate medical treatment to alleviate symptoms and prevent complications.
Manage allergies
If allergies contribute to your sinusitis, work with an allergy specialist to identify triggers and develop a personalized management plan, which may include medications, allergy shots, or environmental modifications.
Practice nasal irrigation
Use saline nasal irrigation devices to help keep nasal passages moist, flush out irritants, and promote proper sinus drainage. This can be particularly beneficial for individuals with chronic sinusitis or nasal congestion.
Adopt healthy habits
Maintain a healthy immune system through regular exercise, a balanced diet, and managing stress levels. These practices can help reduce the risk of sinus infections and promote better sleep.
